Mental health and substance use disorders are the leading cause of disease burden in America. Total health expenditures due to the co-occurrence of medical, mental health and substance use challenges were estimated to be $406 billion in 2017. Most of the costs associated with comorbid conditions stem from a lack of services integration, leading to poor health outcomes and high economic costs. This presents a potential for improved patient outcomes and substantial savings through the integration of mental health and substance use treatment with physical medical services to deliver pragmatic interventions that increase access.
General Health Integration Learning Collaborative
In April 2021, Montefiore Care Management Organization, in partnership with the National Council for Mental Wellbeing Center of Excellence for Integrated Health Solutions (CoE-IHS), launched a learning collaborative to assist community mental health and substance use service organizations with optimizing whole person care through implementing General Health Integration (GHI) in their organizational programs. Using Advancing Integration of General Health in Behavioral Health Settings: A Continuum-based Framework, a novel evidence-based framework for GHI, participants learn from each other and experts about key evidence-based practices to advance integration, pilot local interventions to improve general health screening and outcomes and share best practices and implementation strategies. Learn more about the learning collaborative by reviewing the mid-year findings.
Who is involved?
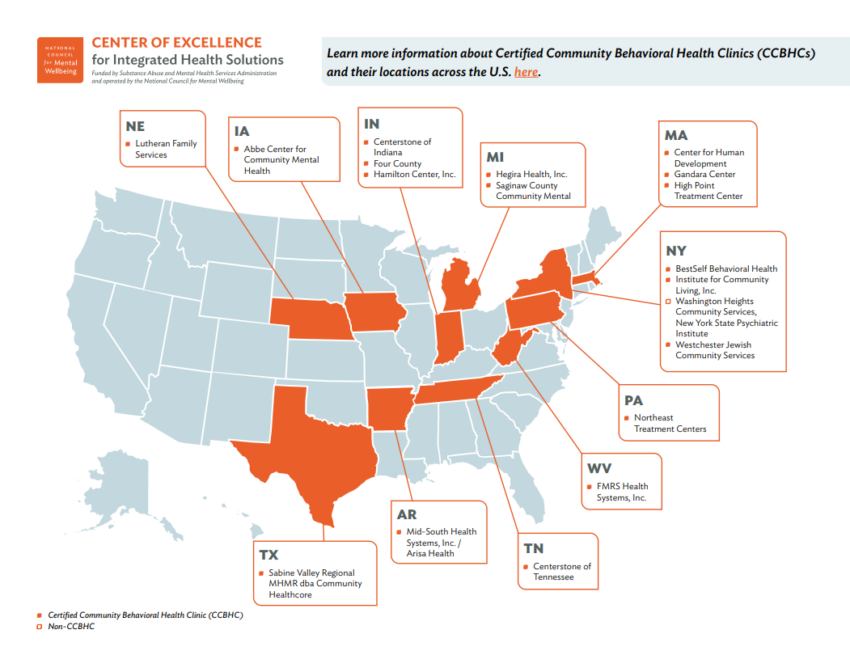
Nineteen mental health and substance use treatment organizations across 11 states were selected to participate from a pool of national applicants. Most participating organizations are Certified Community Behavioral Health Clinics (CCBHC) with varying levels of integration and quality reporting capabilities. In total, the organizations serve an average of 67,600 patients and are able to identify higher risk patients with comorbid physical health conditions. These clinics are providing mental health and/or substance use disorder treatment services with some prior experience integrating a range of general health initiatives into their clinical practice.
To be eligible to participate in this learning collaborative, clinics were required to have an electronic health record system in use for at least one year, committed clinical and administrative leadership with a vision for advancing general health integration and a practice transformation team comprised of at least three individuals (a clinical/executive leader, a member providing care management and a prescriber such as an M.D., D.O., nurse practitioner [NP] or physician assistant [PA]).
Reporting Requirements and Metrics
A key aspect of this learning collaborative is reporting on nine quality metrics that were selected from CCBHC recommended measures and related to key evidence-based practices aligned with the GHI framework. These measures include access to prevention and ambulatory health care; performing screenings for diabetes, tobacco use and cessation, unhealthy alcohol and drug use; screening and treatment monitoring for depression; and screening for social needs, as well as providing brief intervention after screenings. Moreover, organizations have committed to completing baseline and endpoint surveys on their evolving state of general health integration. This data will be used to measure advancement of integration among the participating organizations and support value-based payment models that include GHI advancement.
Mid-year Findings
Recently, the learning collaborative faculty team completed a midpoint progress review for the first five months of the learning collaborative, April – August 2021. Early results indicate that organizations have improved performance in two important ways. First, organizations are increasing the number of measures they report, as well as the completeness of the measures reported. Second, organizations are improving their quality of care, with an average improvement in performance of 5.8% per measure. The measure with the greatest average improvement across programs was screening for social needs with a 15.4% increase over baseline in the first five months.
The diabetes screening measures, had a small decline of 1.4% on average across sites to a sizable decrease for one organization, but seven of nine sites reporting had improvement in this measure at five months. These promising indicators suggest that organizations are making changes in infrastructure and workflows that improve quality of care and data reporting, both of which are critical to sustainability of integration investments.
Evaluation and Impact
An important parallel goal of this collaborative is to evaluate the utility and validity of the General Health Integration framework. Results from the pilot will enable clinicians, payers and state regulatory bodies to better understand and support new ways to incentivize and support organizations that are implementing integration. Finally, we expect that policymakers and clinicians will help disseminate these findings more broadly and use the GHI framework to both improve patient care and encourage payers to support value-based payment models.
Early anecdotes from a few participating organizations include:
- “Participation in the learning collaborative has allowed us to assess the capacity of our current systems to record and report on key measures for individual client care and for overall program performance. One lesson from our participation in the learning collaborative has been that our care teams need systemic reminder mechanisms to ensure the timely and routine collection of assessments for depression, social determinants of health, substance use and more, and that without such reminders clinicians risk losing track of completion of these assessments. To achieve this, we have invested significant effort in exploring mechanisms within our electronic health system for setting reminders on clinician dashboards for when a particular client is due for initial or follow up assessment. This effort has significant pay-off, resulting in our reaching a point recently where more than 85% of our clients have a completed depression screening in the last year and we plan to continue to apply the same approach to the collection of other assessments central to the care of our clients and management of our system of care.”
– William Mullane, D., Director of Innovation, Integration and Community Partnerships, Westchester Jewish Community Services, New York - “Our CCBHC staff and administration have been witness to the positive outcomes of the program enhancements provided through this [learning collaborative] opportunity. One of our clients was going through a transition with his treatment team while receiving a devastating medical diagnosis from the Ga̒ndara PCP. The client relied on the CCBHC team for support and they were able to assist the client by connecting them with a new clinician, new prescriber and a community support program case manager. Months later, the client was approved for social security, was able to get their own apartment, have priority transportation to and from all their appointments and have the needed support of the PCP and clinician to work through their medical diagnosis and mental health matters. The learning collaborative and GHI framework’s guidance on care management and team-based care was what made this case so successful. Not all of this would have been possible so quickly without the support of the Ga̒ndara CCBHC team and added services of being a CCBHC facility.”
– Rahiza Gallardo-Vazquez, Ph.D., Senior Director of Behavioral Health Services, Ga̒ndara Center, Massachusetts
The mid-year findings demonstrate the successes of the 19 participating organizations and their advancement of GHI to date. These findings indicate the likelihood of achieving desired outcomes and meeting intended goals by the end of the learning collaborative, which are to improve upon quality medical care through critical risk factor screening and early detection, monitoring of chronic illness indicators, improved linkages to care and patient education and self-management.
Participant feedback supports the intended utility of the evidence-based framework and captures real-time progress of each organization working to advance general health integration. As participating organizations continue to gather through this learning collaborative, report on quality metrics, learn together and share best practices and implementation strategies to advance general health integration, improved patient outcomes are expected to follow.
Guest Authors
Molly Finnerty, MD
Matt Goldman, MD
Henry Chung, MD

